Immunotherapy
The body’s immune system
An effective treatment for cancer
The healing of cancer has so far been closely linked to the body’s own immune system. Even after the removal of a localized tumour, such as a bladder carcinoma, microscopically small tumour cells remain throughout the patient’s body. These cells, which cannot be imaged, remain untreated and can remain inactive in the body for years and decades, later serving as the basis for the growth of metastases and larger tumor cell clusters. Most men with bladder cancer die from metastases and not from the primary tumor in the bladder.
Nevertheless, conventional therapies for bladder cancer are mainly aimed at treating the primary tumor. Surgery, radiotherapy and chemotherapy even damage the immune system instead of strengthening it. Systematic treatment of the cancer cells scattered throughout the body has not yet been carried out.
Immunotherapy
As support for the body’s own immune system in the fight against tumor cells
It has long been known that there are anti-cancer therapies that support the body’s own immune system in fighting off tumor cells. These procedures are characterized by their ability to kill tumour cells through apoptosis and necrosis. These include techniques such as irreversible electroporation (IRE), reversible electroporation (ECT = electrochemotherapy) and photodynamic therapy (PDT), the latter being an older procedure that has been well researched with regard to its antitumor immune effects1.
INCREASING THE RECOGNIZABILITY OF BLADDER CANCER FOR THE IMMUNE SYSTEM
The immune system recognizes tumours via special tumour antigens that are located on the surface of the tumour cells. In tissue ablation procedures such as IRE, ECT and PDT, these tumor antigens are released in large quantities and recognized by the immune system – comparable to a vaccination in which inactive viruses are injected.
This makes it possible to make tumors that are difficult for the immune system to detect, such as bladder cancer, “visible”.
Strengthening the immune response THANKS to immunotherapy
The resulting immune response against the tumor and cancer cells distributed throughout the body can be intensified by immunotherapeutic agents. Various substances play a role here.
It has been known for around 100 years that simultaneous inflammation with tumors can lead to spontaneous regression1. An established standard therapy for bladder tumors is the induction of an infection with the tuberculosis vaccine Bacillus Calmette-Guérin (BCG). In addition, oncolytic viruses2, dendritic cells, cytokines such as interleukin-6 and the inhibition of T-regulatory cells by low-dose cyclophosphamide3 can enhance the immune response against tumor cells.
Modern immunotherapeutic agents such as check-point inhibitors (e.g. PD1 inhibitors – Keytruda©) have a more targeted effect by strengthening the body’s immune response by blocking certain receptors.
Talk to us on 069 50 50 00 948 or send us an e-mail using the contact form.
VITUS CLINIC FOR COMPLEMENTARY MEDICINE
Innovative integrated therapy concepts for improved survival rates in bladder cancer
At the VITUS Clinic for Complementary Medicine, we use modern immunotherapy approaches to treat bladder cancer not only locally in the bladder, but throughout the entire body. Our aim is to prevent the formation of metastases and tumor recurrence.
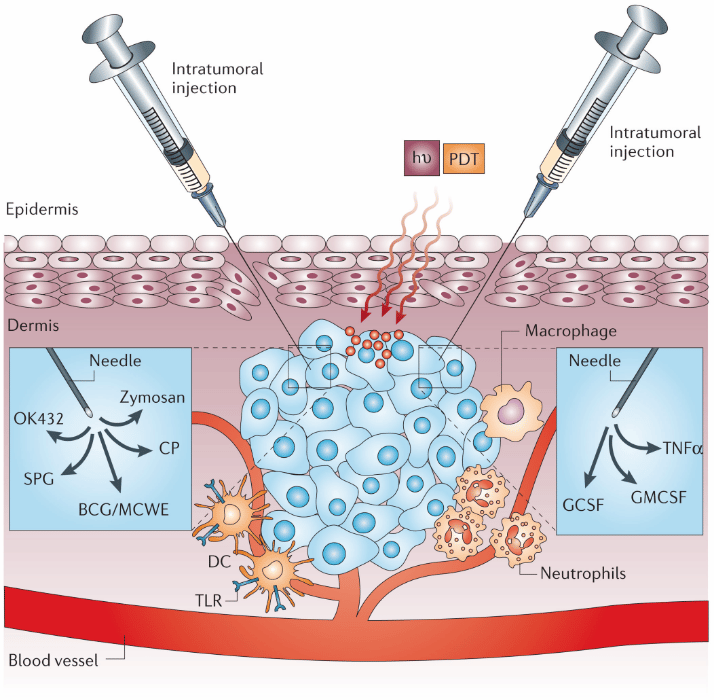
The illustration shows the combination of treatment of a primary tumor (here with PDT) with immunostimulants. The intratumoral injection of various Toll-like receptor (TLR) ligands such as Bacillus Calmette-Guerin (BCG), Mycobacterial cell-wall extract (MCWE), OK432, Zymosan, Schizophyllan (SPG) or Corynebacterium parvum (CP) effectively activates dendritic cells (DCs) and increases antigen presentation and local inflammation. The injection of various cytokines such as granulocyte-macrophage colony-stimulating factor (GMCSF), granulocyte colony-stimulating factor (GCSF) and tumor necrosis factor-α (TNFα) leads to increased infiltration by macrophages, activation of neutrophils and direct destruction of the tumor vessels.

