Photodynamic therapy for breast cancer
Photodynamic therapy (PDT) destroys cancer cells without significantly damaging healthy cells.
Breast cancer differs from normal glandular tissue in the breast in that it grows uncontrollably. An ideal cancer therapy would be able to distinguish cancer cells from healthy cells, locate them and selectively destroy them without damaging healthy cells.
This was previously not possible. Although radiotherapy and chemotherapy have a stronger effect on cancer cells, they damage healthy cells to a very considerable extent. This is why these therapies are applied “fractionally”, in several sessions, to give healthy cells a chance to recover.
Photodynamic therapy (PDT) uses natural dyes and light to gently destroy cancer cells. The dyes are called “photosensitizers” or “photosensitizers” (PS) because they are taken up into cancer cells and make them sensitive to light of certain wavelengths.
When a cancer cell that has taken up the photosensitizer is irradiated with light of a certain wavelength, the light energy triggers chemical processes that lead to the formation of oxygen compounds, especially oxygen radicals, which are highly toxic to cells and kill the cell.
In general, photosensitizers are initially taken up by all cells. But the accumulation of PS in tumor cells is higher than in normal body cells, so that, depending on the type of PS, 10-20 times higher concentrations can be reached in cancer cells. Accordingly, when irradiated with light, tumor cells primarily die off, while normal cells survive.
PDT stimulates the immune system and inhibits the formation of metastases
Depending on the PS and type of treatment, PDT may also damage blood vessels in the tumor, cutting off the blood supply to the tumor, without which the tumor cannot grow.
In addition, PDT triggers an immune response against the tumor cells by causing the dying tumor cells to release tumor antigens that are recognized by the immune system – similar to a vaccination. These tumor antigens enable the killer cells of the immune system to find and destroy the tumor cells throughout the body.
This immune reaction can be strengthened by modern drugs, so-called immunotherapeutics, and, in contrast to chemotherapy, acts selectively on the cells of the treated tumor.
Recent research results indicate that this can inhibit or even prevent the formation of metastases.
How is photodynamic therapy performed?
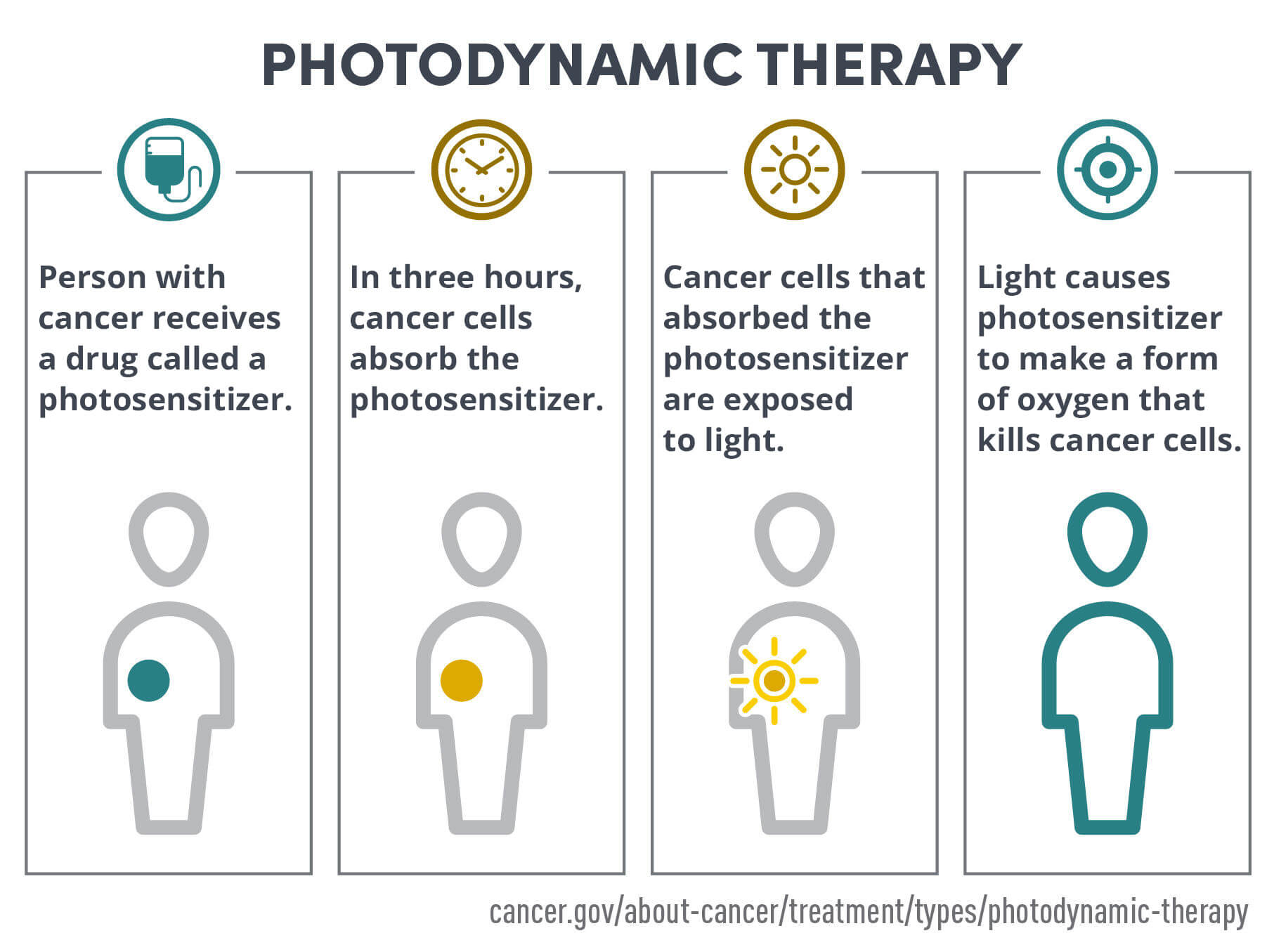
PDT is a two-step process.
In the first step, the photosensitizer (PS) is applied. This is usually done by intravenous infusion, but can also be done by local injection into the tumor.
A few hours later, the photosensitizer has accumulated in the cancer cells. In healthy cells, the concentration of PS is already very low at this point, as it has either been broken down by metabolic processes or excreted from the cell by the cell’s transport mechanisms.
In the second step, thin light guides are placed in and around the tumor in the breast. These are used to illuminate the tumor and the surrounding tissue with laser light of a specific wavelength. The light is absorbed by the photosensitizer (PS), which activates the PS. The activated PS destroys the cancer cell.
Due to the selective accumulation in the cancer cells, primarily the tumor is destroyed, while normal tissues and cells are spared.
Chlorin E6 – a natural photosensitizer based on the plant pigment chlorophyll
While some of the older photosensitizers damage cancer cells and healthy cells at the same time, it has been shown that PS Chlorin E6 accumulates specifically in tumor tissue. Green porphyrin is made from natural plant substances 1 .
Chlorin E6 accumulates 20-fold more in tumor tissues than in healthy cells. If the tumor cells are then irradiated with monochromatic laser light with a wavelength of 665 nanometers – red light – the energy of the laser light is transferred to the chlorin E6 molecule.
The absorbed energy is transferred to oxygen molecules in the cell, creating oxygen radicals with highly reactive singular electrons. These oxygen radicals are highly reactive and react with biological components of the tumor cell such as the nucleus, mitochondria and cell membrane. As a result, the tumor cell loses its function and structure and dies.
Surrounding healthy cells that have not accumulated chlorin E6 remain largely unaffected by the red laser light.
The substance has already been successfully tested in a phase IIb clinical trial for the treatment of central bronchial carcinoma. In the available studies and experiences within the framework of healing trials, Chlorin E6 did not show any serious side effects.

Advantages of photodynamic therapy
PDT primarily destroys tumor cells and spares normal cells and tissue.
In addition, PDT destroys cells without heating, unlike widely used thermal ablation techniques such as radiofrequency ablation (RF ablation) and High-Energy Focussed Ultrasound (HiFU). Thus, PDT preserves the tissue infrastructure of fibers and interstitial matrix, as well as nerves and vessels. This makes it possible to preserve the function of anatomical structures.
Also, PDT minimizes scarring and induces strong secondary immune effects against cancer cells.
Disadvantages of photodynamic therapy
PDT, despite selective accumulation in tumor cells, can also damage normal cells and tissues and cause side effects.
In most cases, the light can only penetrate solid tissue to a depth of about 1 cm during PDT and can only destroy cells to this depth. When treating solid tumors of larger dimensions, many light sources – usually fiber optic light guides – must be inserted into the tumor at intervals of 1 cm to illuminate the entire tumor mass.
Potential side effects
The damage to normal cells caused by PDT, although limited, can lead to temporary swelling and pain and, in rare cases, scarring in the treatment area.
For which patients is therapy suitable?
In contrast to surgical, chemotherapeutic or radiotherapeutic procedures, photodynamic therapy (PDT) is significantly less stressful for the patient.
Although there are no clinical studies to date that show in which cases of breast cancer photodynamic therapy is particularly suitable, it can be deduced from the lower side effects of PDT that it is particularly suitable for the treatment of breast cancer if the woman concerned wishes to minimize the side effects of the treatment.
PDS is also a gentler alternative to radiation and/or chemotherapy for difficult-to-treat recurrent tumors and skin metastases.
PDT also represents a therapeutic problem-solving alternative for patients who are considered “out of treatment” in the “conventional medical sense” or for patients who reject conventional therapies.
Of particular importance is the fact, now scientifically confirmed, that PDT activates the body’s own immune system in the fight against breast cancer cells and that metastases can thus be avoided or treated more effectively. These immune effects can be further enhanced by modern immunotherapeutic agents.
Other cancers and precancerous lesions treated with photodynamic therapy
The U.S. Food and Drug Administration (FDA) has cleared photodynamic therapy for the treatment of the following conditions:
- Actinic keratosis
- Advanced cutaneous T-cell lymphoma
- Barrett esophagus
- Basal cell carcinoma of the skin
- Esophageal Cancer
- Non-small cell lung cancer
- Squamous cell carcinoma of the skin (stage 0)
PDT is also used to relieve the side effects of the following cancers (palliative, not curative).
- Esophageal cancer when it blocks the esophagus
- Non-small cell lung cancer when it blocks the airways
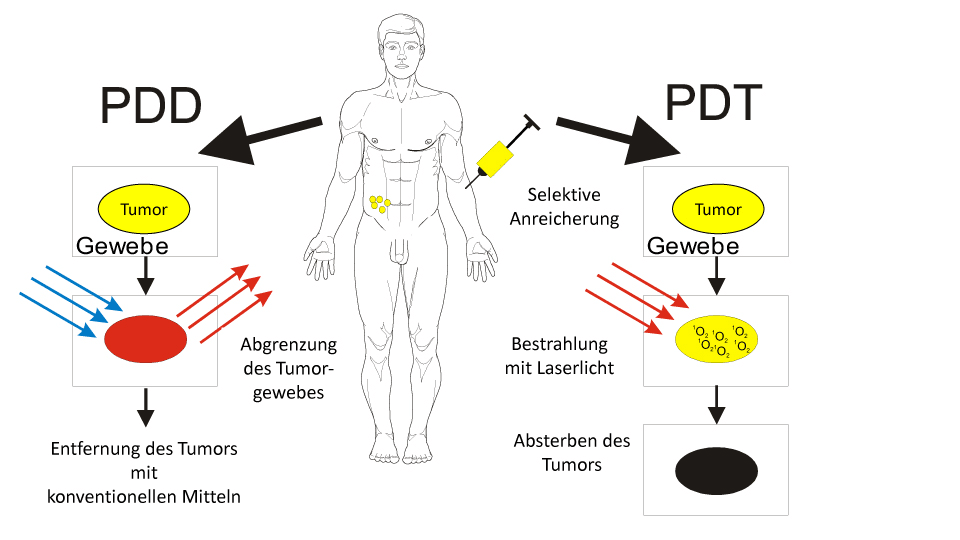
With Chlorin E6, photodynamic therapy (PDT) is also possible afterwards (right part of the figure). Three hours after the injection of Ce6, the tumor cells took up the substance. Irradiation with special laser light triggers a chemical reaction in the tumors, producing singlet oxygen.


